Tag: Functional medicine
-
Are you super sensitive to chemicals, food, light and life?
Maybe you feel like you are allergic or reactive to everything and can’t understand why? There can be lots of different reasons for this but before we go removing this and that and trying to identify multiple triggers I like to ask the question “are your cell membranes working right?” Our cell membranes act as…
-

Staying alive in toxic times
Photo by Demure Storyteller on Unsplash
-

Facts of rice
A lot of my clients rely on white rice or pasta for quick meals. I thought I would write this blog about the benefits of brown rice and how to prepare it. Hoping to convince you all that brown rice is the way forward. Brown rice is a whole grain and a major source of…
-

How to Optimise Your Vitamin D Level
There are two major forms of vitamin D from two different sources. In the UK our main dietary sources of vitamin D are food of animal origin, foods fortified with vitamin D and supplementation. Naturally rich food sources include egg yolk and oily fish such as salmon, mackerel, herring and sardines. Absorption We probably absorb…
-

All about the menopause
Bullet point summary Peri menopause – the window of opportunity Lots of women dread the menopause. It’s often viewed as a process of ageing and associated with uncomfortable symptoms ranging from heavy periods to weight gain, anxiety and night sweats. Lara Biden, author of the ‘hormone repair manual’, reframes this as a “window of opportunity”…
-
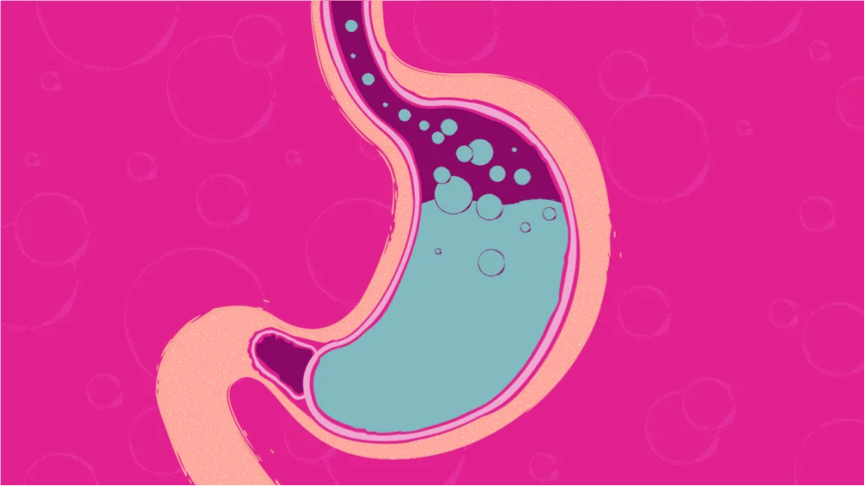
Acid reflux and the problem with PPI’s
Acid reflux is a common and distressing complaint that my clients often need help with. As many as 20 percent of Europe’s population is estimated to suffer from acid reflux – that is 112 million people in Europe alone. In 2019 over 60 million doses of the two most common drugs known as proton pump…
