Tag: nutritional therapy
-
Heart burn, acid reflux, GERD – what is the difference?
All of these conditions occur when acid from the stomach escapes into your oesophagus, via the sphincter at the top of the stomach, creating a burning sensation. All of these painful digestive conditions are related and tend to cause similar symptoms, however, they usually develop in stages. In the case of acid reflux, stomach acid…
-
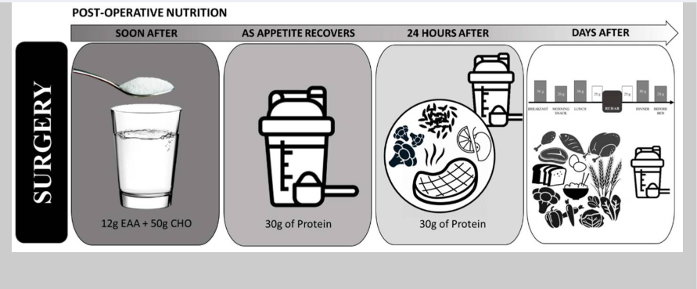
Nutritional support for post-surgery
I frequently support clients who have either had or are going to have operations. It is common knowledge that your nutritional status and health prior to an operation has a big impact on the outcome of surgery and your recovery post operation. It is estimated that between 24% and 65% of patients are malnourished and…
-
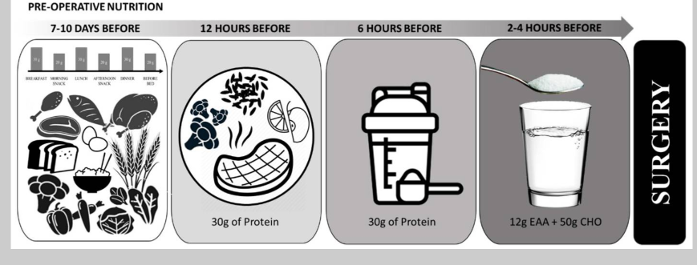
Preparing for surgery with nutritional support
I frequently support clients who have either had or are going to have operations. It is common knowledge that your nutritional status and health prior to an operation has a big impact on the outcome of surgery and your recovery post operation. It is estimated that between 24% and 65% of patients are malnourished and…
-

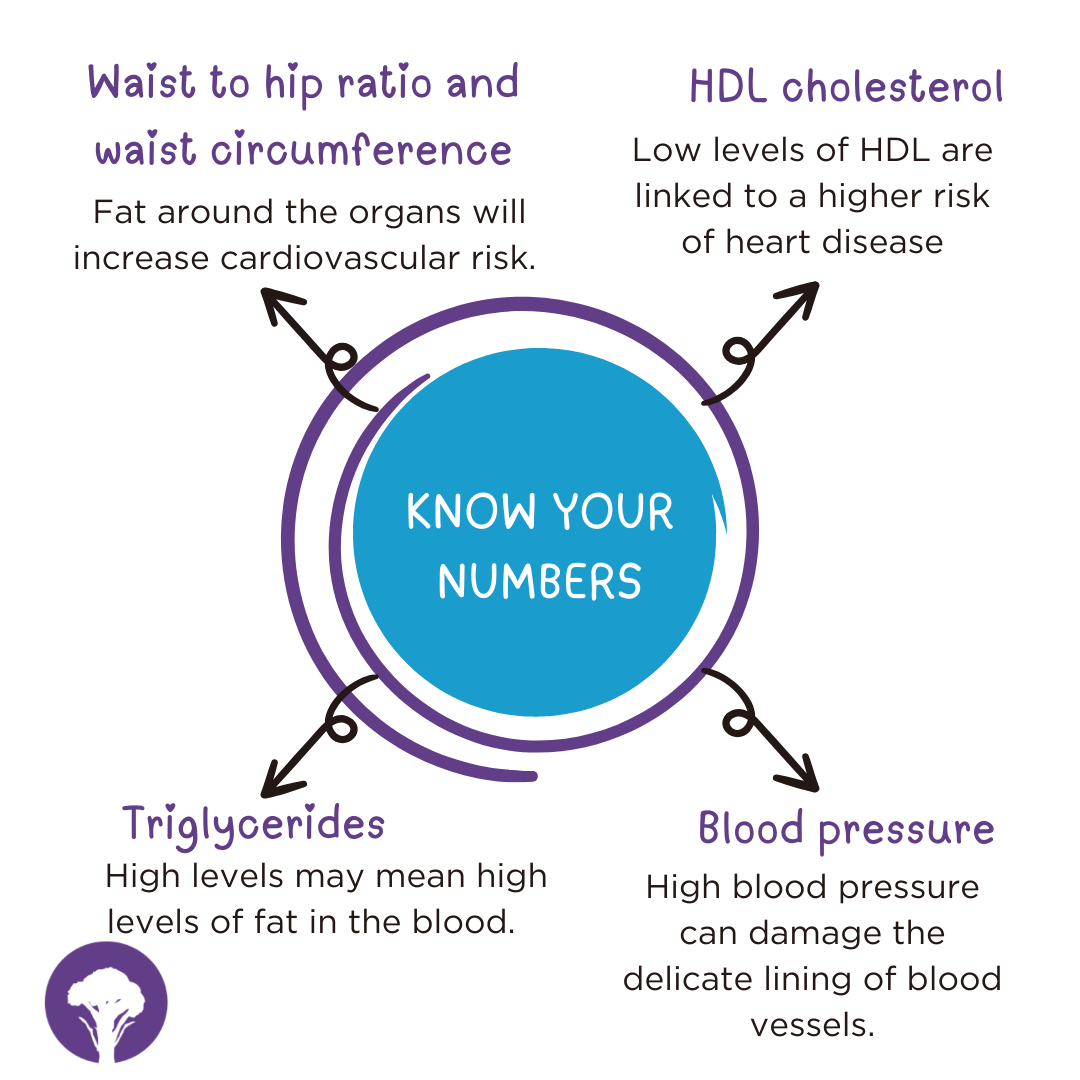
What do Nutritional Therapists help with and how to find one?
You might be someone who gets bloated after every meal. Or someone who feels exhausted by mid-morning despite a full night’s sleep. Maybe your skin flares up regularly, or you’re dealing with unpredictable mood or energy changes. These are just a few of the reasons people turn to nutritional therapists. Common concerns supported by nutritional…
-

Silent reflux – what is this?
Over 112 million people in Europe, about 20% of the population, are estimated to suffer with acid reflux. Acid reflux occurs when acid from the stomach flows back up into the tube running from the throat to the stomach (the oesophagus). This causes a burning sensation known as acid reflux or heart burn. Silent reflux…