Tag: nutritional therapy
-
What fats can I cook with?
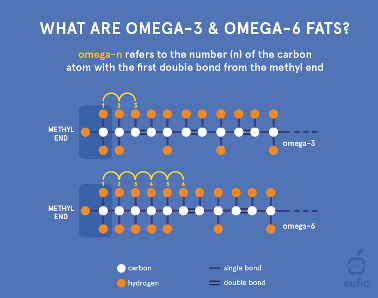
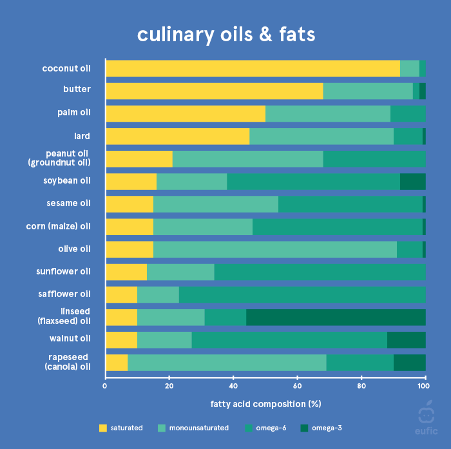
This blog is a reminder of which fats to use for cooking and which ones are best used cold in salad dressings. It also covers which ones to avoid. Fatty acids are classified according to the presence and number of double bonds in their carbon chain. Saturated fatty acids (SAFA) contain no double bonds, monounsaturated…
-
Are you super sensitive to chemicals, food, light and life?
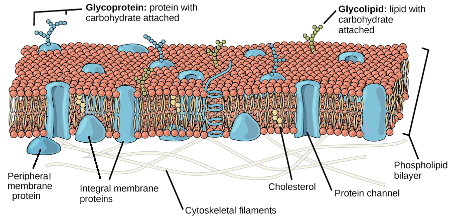
Maybe you feel like you are allergic or reactive to everything and can’t understand why? There can be lots of different reasons for this but before we go removing this and that and trying to identify multiple triggers I like to ask the question “are your cell membranes working right?” Our cell membranes act as…
-
Do your cells need an oil change?
Today’s modern diets can often mean we eat too much or too little fat, or frequently just the wrong type. Our cell membranes consist of lots of oil aka. fat. For optimal performance they require quite a specific ratio of different types of fats, especially with regard to the essential fatty acids (EFA’s), omega 3…
-

10 super healthy switches to boost nutrition
Here’s some simple easy changes to boost your nutrition. Check my website for recipes and to sign up to my newsletter.
-

Staying alive in toxic times
Photo by Demure Storyteller on Unsplash
-

Weight gain! Is stress to blame?
Photo by Fuu J on Unsplash