Tag: nutritionist
-

How to Optimise Your Vitamin D Level
There are two major forms of vitamin D from two different sources. In the UK our main dietary sources of vitamin D are food of animal origin, foods fortified with vitamin D and supplementation. Naturally rich food sources include egg yolk and oily fish such as salmon, mackerel, herring and sardines. Absorption We probably absorb…
-
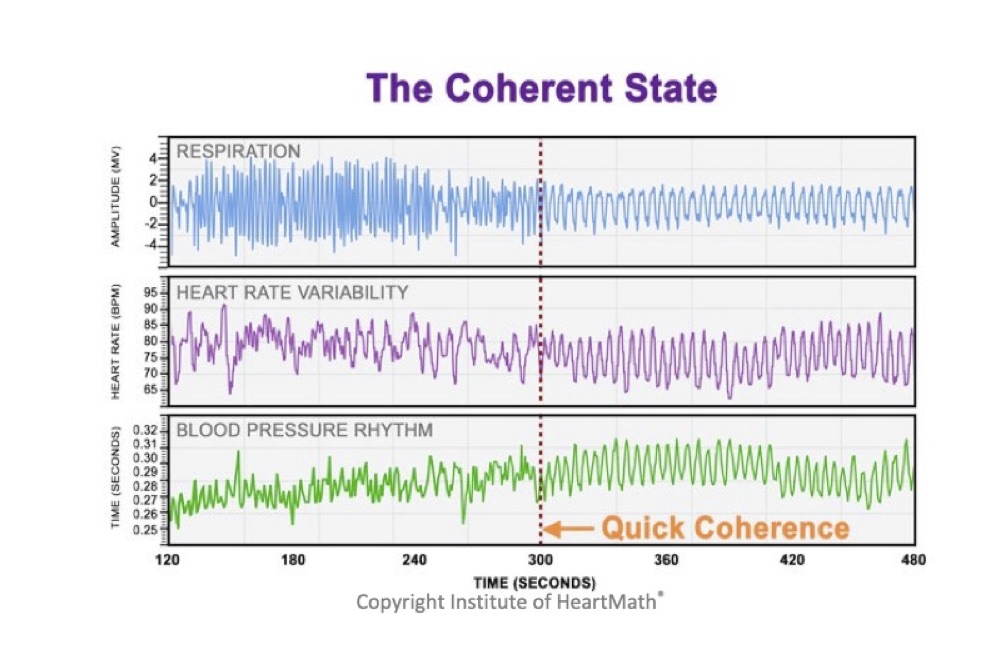
Enter ‘The zone’
An air of mystery surrounds ‘The Zone’, a near mythical state of mind-body alignment which athletes seek but few master. Rupert Sheldrake (author and biologist) suggests that sport may be one of the few remaining ways for people to experience an altered state of consciousness. Sport requires: total concentration on the ‘present’; dedication; discipline and…