Can't lose weight? 10 things to consider
This is a summary of some of the core reasons for why weight loss can be so difficult for some people. It’s a complex area involving biology, physiology, emotions and psychology to name just some. However if you feel like you have tried everything you could have a think about the list below which summarises some of the key areas to address.
Appetite regulation system, poor eating habits and compromised digestion.
This can include things like eating too fast. The satiety hormones take time to register and react to food intake. If we eat fast we can over eat before the feedback mechanism has time to respond and let us know we are full. Similarly, if we eat on the run or with our attention elsewhere such as the computer or TV, studies show that we eat more.
New research is showing that there are more stretch (mechano) receptors in the small intestine than the stomach. They tell the brain we are full via nerve feedback. If digestion is compromised in any way then food will take longer to reach the small intestine. It is now thought that this delays signals to the brain that we have eaten enough and extracted the nutrients we need. So improving digestive function can be part of the solution.
Eating slowly and chewing properly as well as other simple changes to the way we eat can make a big difference here. It takes an effort to change habits which are our default way of thinking about and consuming food. But once you correct them and the new habits are ingrained you can go back onto autopilot, it’s just one that serves you better.
Lack of movement and too few muscle cells.
The more muscle cells you have, the more mitochondria you will have. These organelles are responsible for turning food into energy. The more you have the higher your basic metabolic rate (BMR) will be. This is the amount of calories you burn to maintain your body’s function at rest. It is generally thought that our BMR accounts for 70%+ of our daily energy requirements. So another aspect of weight loss can be adjusting our training schedule to improve mitochondria numbers and function.
Lack of nutrition knowledge and understanding about how the body works.
This can result in a poor quality diet perhaps including a lot of ultra processed food (UPF) or a very low calorie diet and yo-yo dieting. Sometimes we need to keep an eye on portion size and plate content and a calorie assessment can be useful here. However I tend to focus initially on the nutrient and micronutrient content of the diet. Once we get this right and the body is nourished then we can take a look at tweaking plate content and construction. I think a lot of ‘diets’ fail because if the body isn’t nourished properly there maybe micronutrient deficiencies so the body craves food in an attempt to resolve this. This is interpreted as hunger.
There is no one method to lose weight. Different methods suit different people’s lifestyles, individual preference sand health status. To some extent they all work, at least initially. What’s important is to establish a baseline that keeps weight stable and the body healthy. This helps to make the body feel safe. Then we can mix and match different weight loss strategies to get the body to adapt. Remember we want it to do something it wouldn’t naturally want to do, based on evolution, which is to lose weight.
The problem with very low-calorie diets (VLCD) and yo yo dieting is the body does something called adaptive thermogenesis. It adapts to the altered calorie intake. It’s also very hard to maintain these over the long term and it can be stressful for the body. It is not a time to lose weight when we are stressed (see BLOG here https://helenmaxwellnutrition.co.uk/weight-gain-is-stress-to-blame/
Lack of hormetic challenge.
Exposure to hormetic stress builds resilience and occurs when we are challenged without overly exhausting ourselves. It includes such physical activities as high intensity interval training, cold exposure (showers or ice baths) and fasting. It’s the use it or lose it principle. It’s an adaptive response to a challenge generated by the environment. Even our response to drugs is a hormetic challenge of sorts. Modern life has evolved to reduce many of our physical hormetic challenges, think central heating, air conditioning and our indoor lifestyles. There are many simple ways to introduce this such as cold showers, breathwork and exercise.
Poor management of blood sugar.
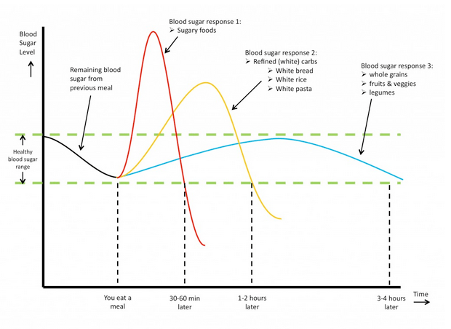
Source: https://www.gestationaldiabetes.co.uk/gestational-diabetes-diet/
This is probably the most useful starting point for most people. You need stable, well managed blood sugar (glucose) if you want to lose weight. If glucose levels in the blood are too high it has to be removed. Insulin takes glucose into the cells to use for energy but if there is no demand it will be taken to the liver where the majority will be stored as fat. Hence insulin is often referred to as the fat storage hormone. So we want to try and keep our levels of insulin low and there are numerous nutritional strategies and supplements that can help with this.
Equally if blood glucose is too low this is stressful for the body. Stress raises cortisol which triggers the release of glucose stores, known as glycogen, from the liver or muscle. Alternatively the body will make glucose by breaking down tissue. Initially this can trigger weight loss but if cortisol stimulation is ongoing, as in chronic stress, this can lead to sustained high blood sugar levels which will necessitate more and more insulin. If the cells become resistant to insulin from stress, poor diet, high sugar intake or poor liver function then insulin resistance can develop which is associated with fat storage (see https://helenmaxwellnutrition.co.uk/weight-gain-is-stress-to-blame/).
Poor thyroid and/or hormone function leading to a dysregulated metabolism.
Our thyroid regulates our metabolic rate which is how we make energy. If thyroid hormone production is low this effectively slows the metabolism causing symptoms such as ‘tired and wired’; anxiety; poor sleep; negativity and depression; shakiness between meals; irritability and a very short fuse. This often leads to abdominal weight gain. This kind of symptom pattern usually requires professional assistance from a qualified nutritional therapist and the medical profession to try to resolve the underlying hormone malfunction. Overproduction of cortisol can play a role in this so stress management is crucial, see below.
Stress and overload.
If the body is chronically stressed then it won’t be able to lose weight. To lose weight requires good digestion, good liver function and good blood sugar and insulin management. All of this requires energy for your internal organs to work properly. Chronic stress takes the energy away from internal function to the extremities, (arms and legs) and the heart so we can run, fight or hide. The body won’t undertake remodelling or restructuring when it’s focused on survival. It’s the same as life. When you are in a stressful life situation you focus on the essentials and the body is the same. You can read more on this here https://helenmaxwellnutrition.co.uk/weight-gain-is-stress-to-blame/
Gut and liver function.
The microbiome (bacteria) in our gut facilitates nutrient extraction from and absorption of food. The importance of nourishing the body in order to lose weight is covered in point 3 above. Most studies seem to point to the ratio of Firmicutes to Bacteroidetes being significantly higher in overweight and obese subjects (Ley, 2010; John and Mullin, 2016). In addition lean subjects appear to have a more diverse and complex microbiome (Kasai et al., 2015; Lv et al., 2019).
The gut microbiota plays a major role in energy generation (metabolism) from the fermentation of fibre and protein in the colon to produce short chain fatty acids (SCFA’s). SCFA’s affect body weight, glucose regulation and insulin sensitivity as well as playing roles in satiety and appetite. Hence the microbiome impacts weight in a number of complex ways through influencing food intake (type and quantity), gut microbiota, nutrient levels and metabolism.
Liver function is critical to maintain a healthy weight. It plays a major role in managing blood sugar (see 5). It controls the the conversion of excess glucose to fat and the breakdown of fat for energy. If liver function is impaired then this system can struggle, fat metabolism deteriorates, and as a result fat accumulates in the liver. This can lead to non-alcoholic fatty liver disease (NAFLD) and/or weight gain. The liver is of course the major detoxification organ of the body. If it malfunctions toxins can build up which can interfere with hormone function and affect metabolism, which often leads to weight gain.
Good gut and liver function are therefore key for successful weight loss. Focusing on improving both of these is often a significant part of any weight loss programme.
Sleep.
Modern lifestyles often mean insufficient sleep. Insufficient sleep causes stress which has already been discussed above. Stress and lack of sleep can lead to comfort eating which tends to be carbohydrate. This can easily become a vicious cycle as carbohydrates, if not wholegrain or good quality, elevate blood glucose quickly. This triggers a lot of insulin very quickly followed by a sudden drop which results in low blood glucose (hypoglycemia) and we end up with poor management of blood sugar (see 5).
The association between lack of sleep and being overweight is well known and shift workers are a prime example of this. Ideally we need 8-9 hours of sleep between 9:30pm and 6:30am. The emerging science of how circadian rhythm interacts with nutrition and health is called chrononutrition and adapting meal timing and structure to take account of our circadian rhythm can really help support weight loss and health.
Change and the brain.
Losing weight involves change on many levels and the organ of change is the brain. It contains the most neurons and the greatest potential to create change. There will often be a lot of negative thinking and slef around excess weight. We have 50-60 thousand thoughts a day and most are the same as the day before. To lose weight we want to start interrupting these thought patterns and changing our focus from what we don’t want, to what we do. Pictures of how you want to look, vision boards to remind you of your goals, even just taking a few minutes each day to tune into how you want to look and feel. Working with other therapists can help such as CBT, NLP, hypnotherapy, whatever it takes to keep on the right track. If meditation is your thing then Dr Joe Dispenza offers many options and this link talks about the brain and how to change https://www.youtube.com/watch?v=EpOMk1jOzgk&t=47s
References
Aoun, A. (2019) The Influence of the Gut Microbiome on Obesity in Adults and the Role of Probiotics, Prebiotics, and Synbiotics for Weight Loss. Cell: 179: pp.1129-1143. https://doi.org/10.1016/j.cell.2019.10.031
Bai, L. et al (2019) Genetic Identification of Vagal Sensory Neurons That Control Feeding. Cell: 179(5) pp1129-1143. doi:https://doi.org/10.1016/j.cell.2019.10.031
Kasai, C. et al. (2015) Comparison of the gut microbiota composition between obese and non-obese individuals in a Japanese population, as analyzed by terminal restriction fragment length polymorphism and next-generation sequencing. BMC Gastroenterology: 15(100). doi: 10.1186/s12876-015-0330-2
Muller, M.J. et al. (2016) Changes in Energy Expenditure with Weight Gain and Weight Loss in Humans, Current Obesity Reports: 5(4): pp. 413-423. doi: 10.1007/s13679-016-0237-4
Rattan, S.I.S and Demirovic, D. (2010) Hormesis can and Does Work in Humans. Dose-Response: 8(1) pp.58-63. doi:10.2203/dose-response.09-041.Rattan
https://www.nhlbi.nih.gov/news/2023/chrononutrition-timing-meals-matters-your-health